9-1-1: Older Adults with Dementia Need Better Care in America’s Fast-Paced Emergency Rooms
December 17, 2024Local emergency rooms are often the first and last places older adults with Alzheimer’s disease and their caregivers turn to for care either because their options have run out or they feel they have nowhere else to turn. Both can be true at the same time, and sadly when it comes to dementia, it often is.
The problem though is that while ERs are effective at handling medical emergencies, they are not as adept in managing the complex and long-term needs of patients with dementia who are increasingly and repeatedly showing up in these fast-paced and disorienting environments, and some are getting admitted for lengthy hospital stays, even when avoidable.
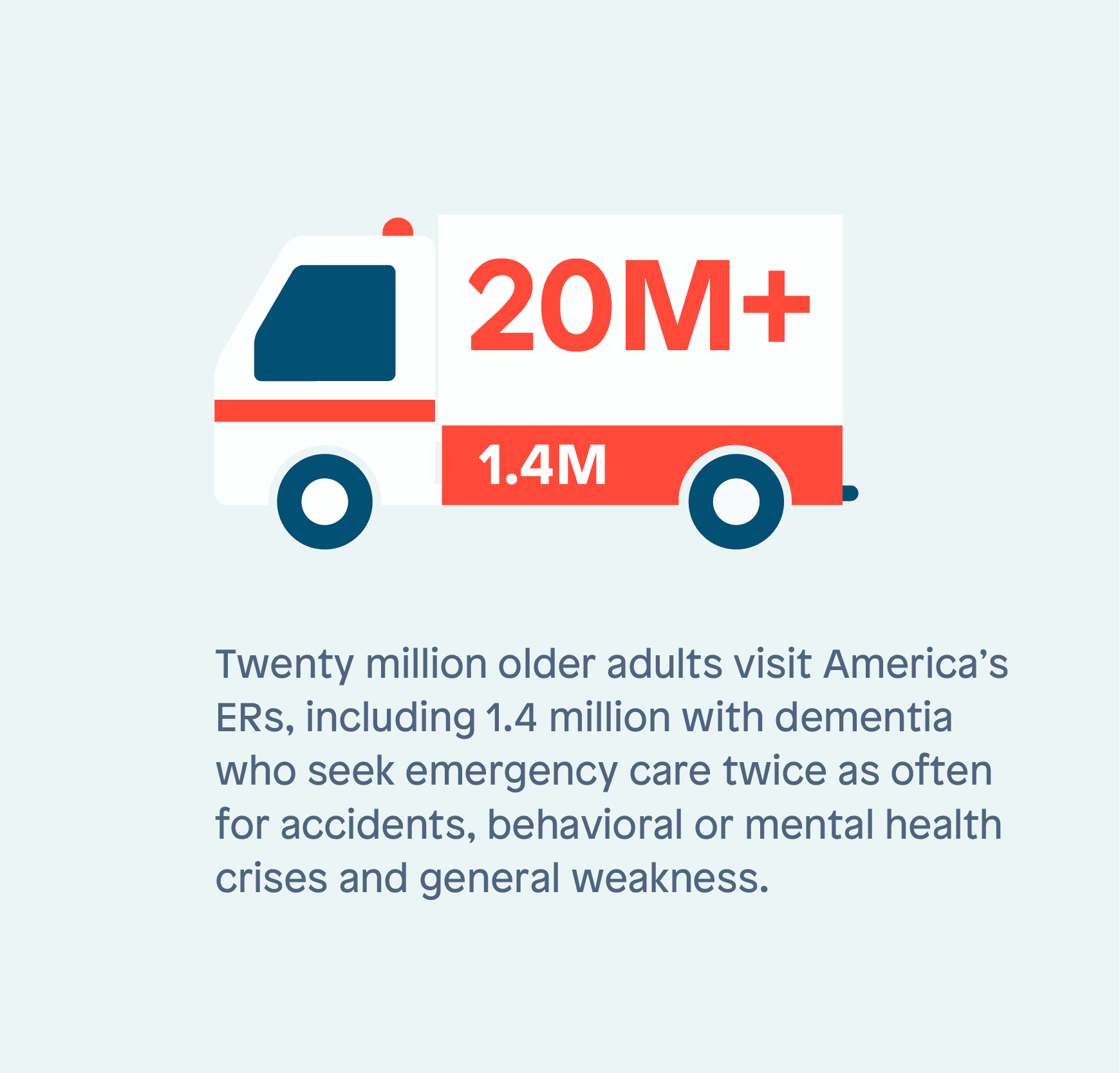
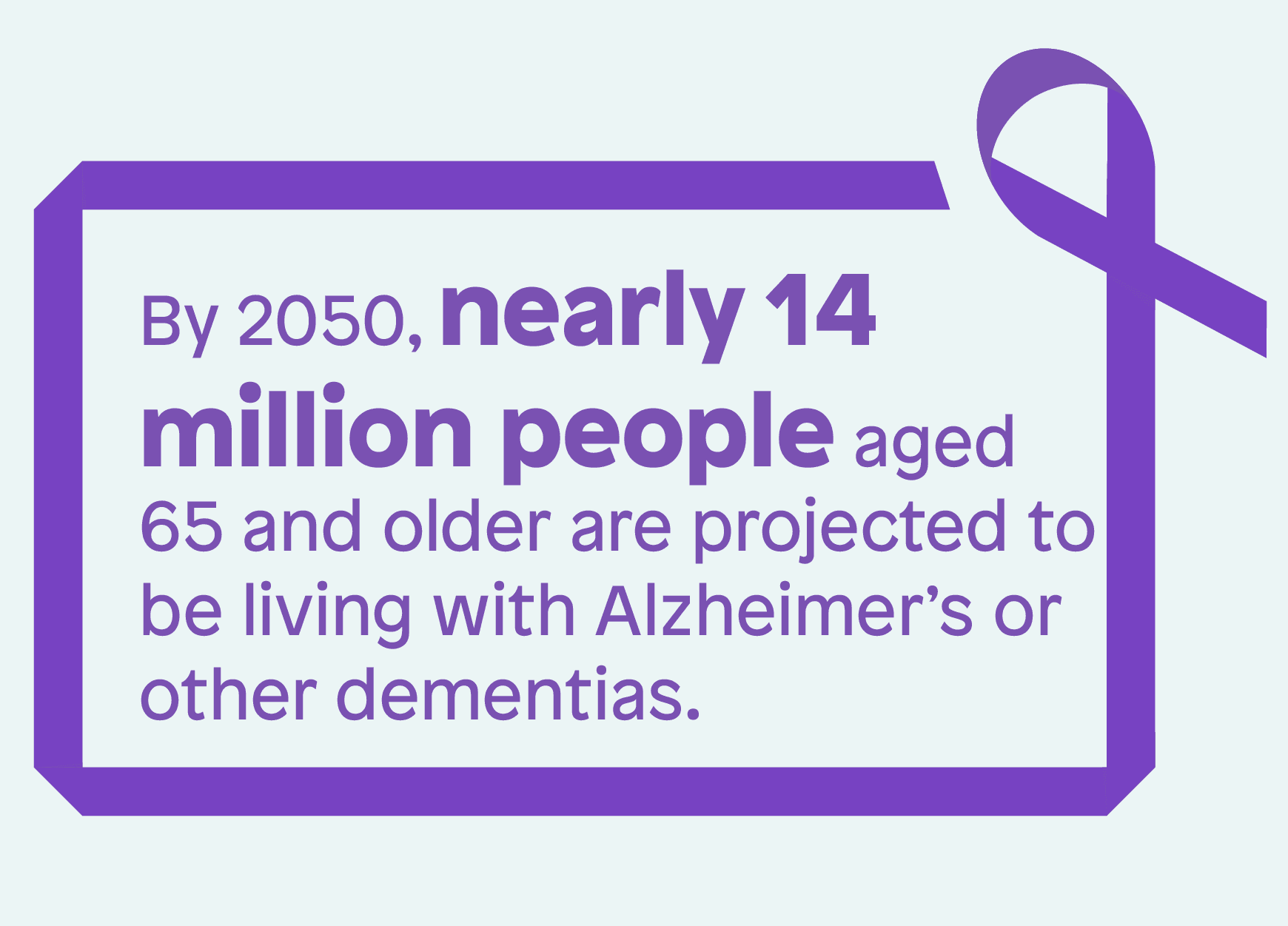
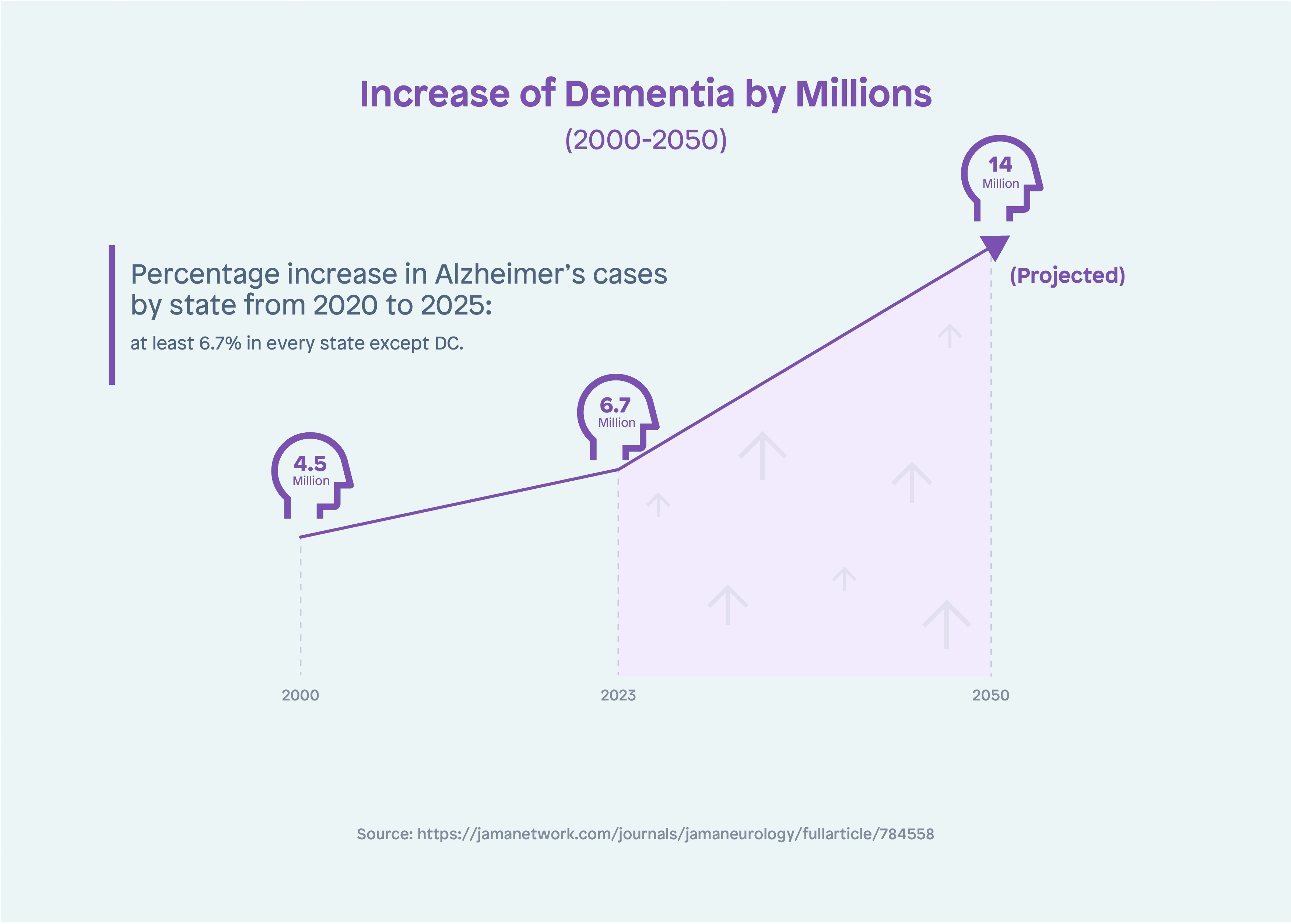
Each year, more than 20 million older adults visit America’s ERs, including 1.4 million with dementia who seek emergency care twice as often for accidents, behavioral or mental health crises and general weakness. By 2050, nearly 14 million people aged 65 and older are projected to be living with Alzheimer’s or other dementias.
These patients tend to undergo more medical tests and receive prescriptions for antipsychotic drugs at more than twice the rate as other patients over 65, according to a study in JAMA Neurology. Other studies show they are more likely to be admitted to the hospital and incur medical expenses about five and a half times higher than seniors with no dementia.
New treatments that reverse or slow dementia are needed, but with major breakthroughs still on the horizon, geriatric-focused approaches, programs and practices are emerging that spot health and life problems earlier, better coordinate physical health, mental health and social services, and treat older patients with or without dementia more holistically, rather than one emergency at a time.
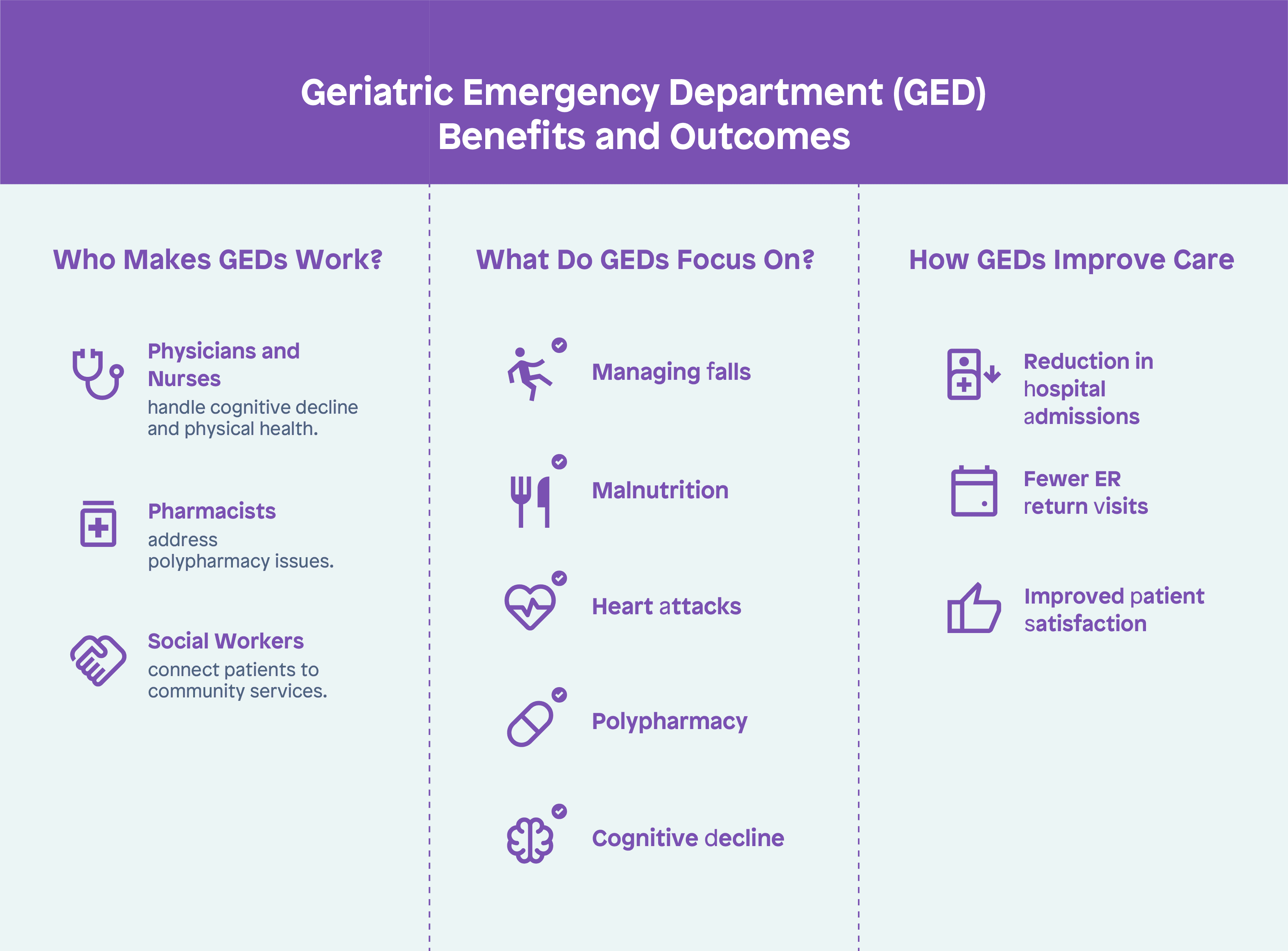
Geriatric emergency departments (GEDs) for one are increasing throughout the country. While not set up exclusively for dementia workup, these facilities provide specialized emergency care on everything from accidental falls, malnutrition, and heart attacks to age-related issues related to polypharmacy, fragility, and cognitive decline in a senior-friendly environment. Even more importantly, data shows GEDs help improve clinical outcomes, reduce hospitalizations and return visits to the ER, and improve patient satisfaction.
Physicians, nurses, pharmacists, physical therapists, and social workers trained in geriatrics are better able to deal with some of the behavioral aspects of dementia such as anxiety, confusion, and agitation that can be exacerbated in unfamiliar environments. They also pay careful attention to discharges and transitions to home and can reach into the community as needed to connect patients with essential support services.
The GED movement began in 2018, when the American College of Emergency Physicians (ACEP) established the Geriatric Emergency Department Accreditation Program to address the healthcare needs of older persons in the ER and not take a one-size-fits-all approach to care. West Health, a nonprofit focused on healthcare and aging, and The John A. Hartford Foundation provided financial support and foundational work for the program.
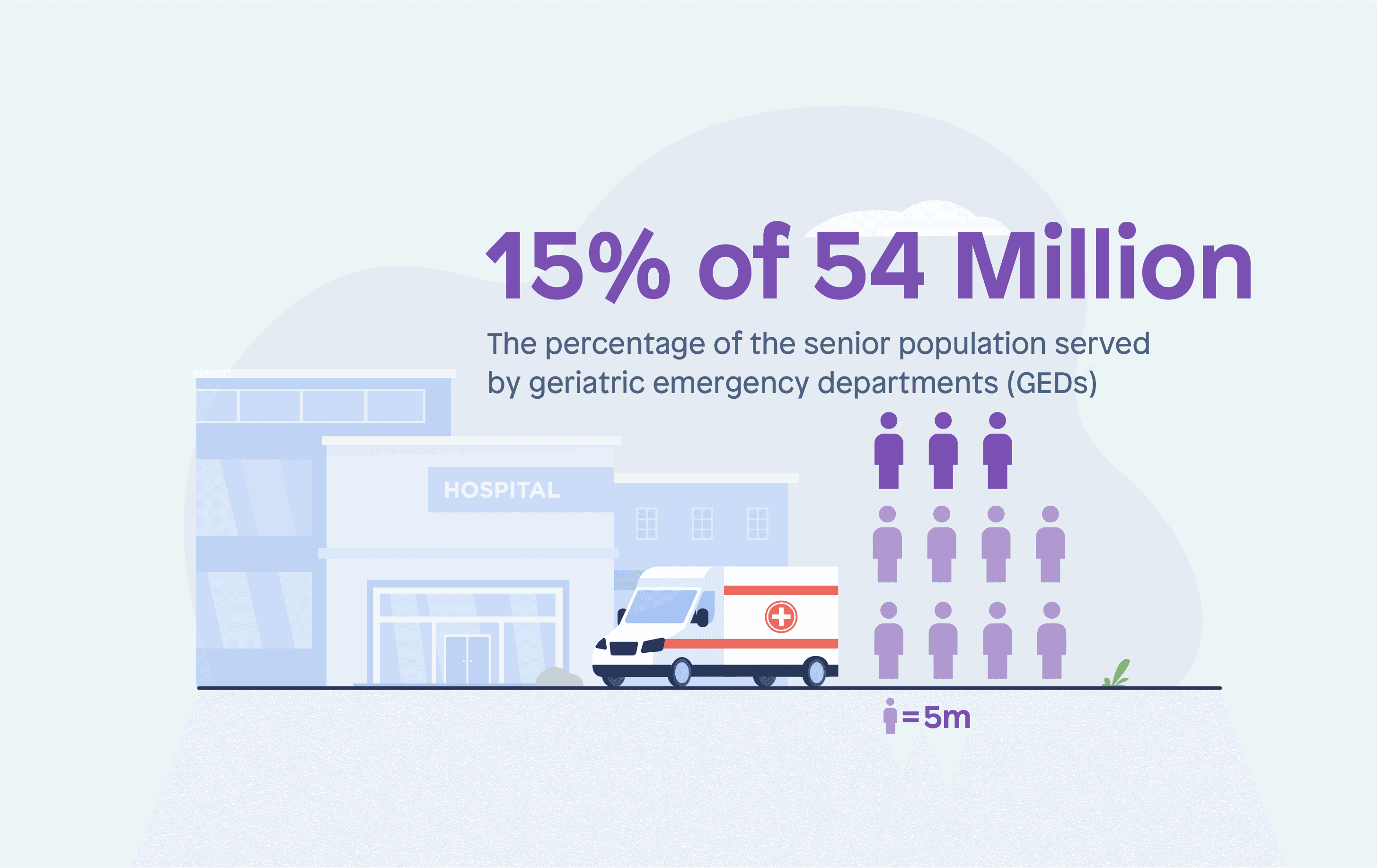
In six years, GEDs grew from a handful in number to more than 500 accredited centers nationwide, that can serve about 15% of the nation’s 54 million seniors, a major capacity issue that will only worsen. The Geriatric Emergency Department Collaborative (GEDC), a worldwide collaborative of healthcare professionals, systems, and organizations, offers resources and took kits to help hospitals establish GEDs in their own communities. GEDC is supported by the John A. Hartford Foundation and the West Health Institute.
According to estimates, older adults will be more than 20% of the population (74 million people) by 2030 and will outnumber people 18 and under for the first time in history. Based on projections, between 2020 and 2025 every state (except DC) will experience an increase of at least 6.7% in Alzheimer’s.
While cardiovascular disease (CVD) and diabetes mellitus (DM) have traditionally been among the leading causes of morbidity and mortality in older adults, dementia is now surpassing them and other chronic conditions.
This means more trips to the ER for older patients with dementia, but if it’s to a GED, a trip here may provide a better framework, even a temporary hub, to guide and support these patients and their caregivers not only during a medical emergency, but also in between, to help prevent emergencies in the first place.